Tags
28 Wednesday Feb 2024
Posted in Depression
≈ Comments Off on The Myth of Low-Serotonin & Antidepressants – Dr. Mark Horowitz
Tags
24 Wednesday May 2023
Posted in brain, Depression
≈ Comments Off on Types of Depression
Tags
Whether you’re a college student in the middle of a major slump, a new mom who can’t pinpoint why she’s feeling so glum, or a retiree grieving over the loss of a loved one, that question isn’t an easy one to answer.
But there’s one thing for sure: “It is much more than just a sad mood,” said Angelos Halaris, MD, a professor of psychiatry and medical director of adult psychiatry at the Loyola University Medical Center in Chicago. Symptoms may include everything from hopelessness and fatigue to physical pain. And just as symptoms vary from person to person, so do the actual diagnoses. The word depression is actually just an umbrella term for a number of different forms, from major depression to atypical depression to dysthymia.
The most common form of depression? Major depression. In fact, about 7 percent of the adult U.S. population has this debilitating mental health condition at any given time, according to the National Institute of Mental Health (NIMH).

If you’re experiencing major depression, you may feel and see symptoms of extreme sadness, hopelessness, lack of energy, irritability, trouble concentrating, changes in sleep or eating habits, feelings of guilt, physical pain, and thoughts of death or suicide — and for an official diagnosis, your symptoms must last for more than two weeks. In some instances, a person might only experience one episode of major depression, but the condition tends to recur throughout a person’s life.
The best treatment is usually with antidepressant medications, explained Dr. Halaris, but talk therapy may also be used to treat depression. And there’s good news: An estimated 80 to 90 percent of people with major depression respond well to treatment.
About 2 percent of the American population has a form of depression that’s less severe than major depression but is still very real — dysthymia.
Dysthymia is a type of depression that causes a low mood over a long period of time — perhaps for a year or more, explained Halaris. “People can function adequately, but not optimally.” Symptoms include sadness, trouble concentrating, fatigue, and changes in sleep habits and appetite.
This depression usually responds better to talk therapy than to medications, though some studies suggest that combining medication with talk therapy may lead to the greatest improvement. People with dysthymia may also be at risk for episodes of major depression.
A whopping 85 percent of new moms feel some sadness after their baby is born — but for up to 16 percent of women, that sadness is serious enough to be diagnosable.
Postpartum depression is characterized by feelings of extreme sadness, fatigue, loneliness, hopelessness, suicidal thoughts, fears about hurting the baby, and feelings of disconnect from the child. It can occur anywhere from weeks to months after childbirth, and Halaris explained it most always develops within a year after a woman has given birth.

“It needs prompt and experienced medical care,” he said — and that may include a combination of talk and drug therapy.
Would you prefer to hibernate during the winter than face those cold, dreary days? Do you tend to gain weight, feel blue, and withdraw socially during the season?
You could be one of 4 to 6 percent of people in the United States estimated to have seasonal affective disorder, or SAD. Though many people find themselves in winter funks, SAD is characterized by symptoms of anxiety, increased irritability, daytime fatigue, and weight gain. This form of depression typically occurs in winter climates, likely due to the lessening of natural sunlight. “We don’t really know why some people are more sensitive to this reduction in light,” said Halaris. “But symptoms are usually mild, though they can be severe.”
This depression usually starts in early winter and lifts in the spring, and it can be treated with light therapy or artificial light treatment.
Despite its name, atypical depression is not unusual. In fact, it may be one of the most common types of depression — and some doctors even believe it is underdiagnosed.
“This type of depression is less well understood than major depression,” explained Halaris. Unlike major depression, a common sign of atypical depression is a sense of heaviness in the arms and legs — like a form of paralysis. However, a study published in the Archives of General Psychiatry (now known as JAMA Psychiatry) found that oversleeping and overeating are the two most important symptoms for diagnosing atypical depression. People with the condition may also gain weight, be irritable, and have relationship problems.

Some studies show that talk therapy works well to treat this kind of depression.
Psychosis — a mental state characterized by false beliefs, known as delusions, or false sights or sounds, known as hallucinations — doesn’t typically get associated with depression. But according to the National Alliance on Mental Illness, about 20 percent of people with depression have episodes so severe that they see or hear things that are not there.
“People with this psychotic depression may become catatonic, not speak, or not leave their bed,” explained Halaris. Treatment may require a combination of antidepressant and antipsychotic medications. A review of 10 studies concluded that it may be best to start with an antidepressant drug alone and then add an antipsychotic drug if needed. Another review, however, found the combination of medications was more effective than either drug alone in treating psychotic depression.
If your periods of extreme lows are followed by periods of extreme highs, you could have bipolar disorder (sometimes called manic depressive disorder because symptoms can alternate between mania and depression).
Symptoms of mania include high energy, excitement, racing thoughts, and poor judgment. “Symptoms may cycle between depression and mania a few times per year or much more rapidly,” Halaris said. “This disorder affects about 2 to 3 percent of the population and has one of the highest risks for suicide.” Bipolar disorder has four basic subtypes: bipolar I (characterized by at least one manic episode); bipolar II (characterized by hypomanic episodes — which are milder — along with depression); cyclothymic disorder; and other specified bipolar and related disorder.
People with bipolar disorder are typically treated with drugs called mood stabilizers.
Premenstrual dysphoric disorder, or PMDD, is a type of depression that affects women during the second half of their menstrual cycles. Symptoms include depression, anxiety, and mood swings. Unlike premenstrual syndrome (PMS), which affects up to 85 percent of women and has milder symptoms, PMDD affects about 5 percent of women and is much more severe.
“PMDD can be severe enough to affect a woman’s relationships and her ability to function normally when symptoms are active,” said Halaris. Treatment may include a combination of depression drugs as well as talk and nutrition therapies.
Also called adjustment disorder, situational depression is triggered by a stressful or life-changing event, such as job loss, the death of a loved one, trauma — even a bad breakup.
Situational depression is about three times more common than major depression, and medications are rarely needed — that’s because it tends to clear up over time once the event has ended. However, that doesn’t mean it should be ignored: Symptoms of situational depression may include excessive sadness, worry, or nervousness, and if they don’t go away, they may become warning signs of major depression.
10 Wednesday May 2023
Posted in Coping Skills, Depression
≈ Comments Off on How to Help Yourself if You Are Depressed
Tags
Depressive disorders can make one feel exhausted, worthless, helpless, and hopeless. It is important to realize that these negative views are part of the depression and do not accurately reflect the actual circumstances. Negative thinking fades as treatment begins to take effect. In the meantime:
12 Wednesday Apr 2023
Posted in brain, Depression
≈ Comments Off on Researchers pinpoint brain’s happiness region
Tags
Happiness is the meaning and the purpose of life, the whole aim and end of human existence,” the ancient Greek philosopher Aristotle once said. But how does one reach this goal? According to a new study by researchers from Japan, a person’s happiness may depend on the size of a specific brain region.
Researchers found people who were happier had larger gray matter volume in the precuneus region of the brain.
Study leader Dr. Wataru Sato, of Kyoto University in Japan, and colleagues publish their findings in the journal Scientific Reports.
The definition of happiness has been debated for centuries. In recent years, psychologists have suggested that happiness is a combination of life satisfaction and the experience of more positive than negative emotions – collectively deemed “subjective well-being.”

But according to Dr. Sato and his colleagues, the neurological mechanisms behind a person’s happiness were unclear.
“To date, no structural magnetic resonance imaging (MRI) investigation of the construct has been conducted,” they note.
“Identification of the neural substrates underlying subjective happiness may provide a complementary objective measure for this subjective construct and insight into its information-processing mechanism.”
Meditation may boost happiness by targeting precuneus brain region
To address this research gap, the team used MRI to scan the brains of 51 study participants.
After the scans, subjects were asked to complete three short questionnaires that asked them how satisfied they are with their lives, how happy they are and how intensely they feel positive and negative emotions.
The researchers found that individuals who had higher happiness scores had larger gray matter volume in the precuneus of the brain – a region in the medial parietal lobe that plays a role in self-reflection and certain aspects of consciousness – than their unhappy counterparts.
What is more, the researchers found that one’s happiness may be driven by a combination of greater life satisfaction and intensity of positive emotion – supporting the theory of subjective well-being.
“These results indicate that the widely accepted psychological model postulating emotional and cognitive components of subjective happiness may be applicable at the level of neural structure,” they add.
These findings, the researchers say, indicate that individuals may be able to boost their happiness through practices that target the precuneus, such as meditation:
“Previous structural neuroimaging studies have shown that training in psychological activities, such as meditation, changed the structure of the precuneus gray matter.
Together with these findings, our results suggest that psychological training that effectively increases gray matter volume in the precuneus may enhance subjective happiness.”

Dr. Sato adds that, while further research is required, these current findings may be useful for developing psychological programs that boost a person’s happiness
21 Wednesday Dec 2022
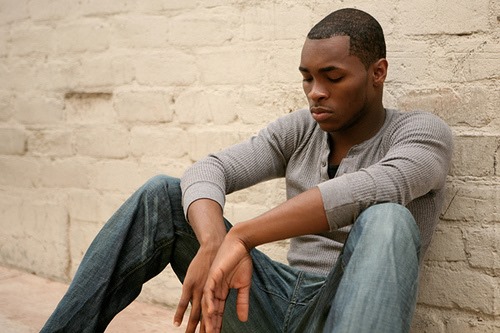
Posted in Depression, Handout, men
≈ Comments Off on Men and Depression
Tags
In my years of facilitating groups I have on occasion facilitated men only groups. One issue that comes up is depression. We all have bouts of sadness now and then and when those bouts of sadness interfere with our daily lives than we need to take a step in the direction of change. Below is part of a handout I often use, particularly with dual diagnosed men.
Symptoms of Depression
Not everyone who is depressed or manic experiences every symptom. Some people experience only a few; some people suffer many. The severity of symptoms varies among individuals and also over time.
· Persistent sad, anxious, or “empty” mood.
· Feelings of hopelessness or pessimism.
· Feelings of guilt, worthlessness, or helplessness.
· Loss of interest or pleasure in hobbies and activities that were once enjoyable
· Decreased energy, fatigue; feeling “slowed down.”
· Difficulty concentrating, remembering, or making decisions.
· Trouble sleeping, early-morning awakening, or oversleeping.
· Changes in appetite and/or weight.
· Thoughts of death or suicide, or suicide attempts.
· Restlessness or irritability.
· Persistent physical symptoms, such as headaches, digestive disorders, and chronic pain that do not respond to routine treatment.

Co-Occurrence of Depression with Other Illnesses
Depression can coexist with other illnesses. In such cases, it is important that the depression and each co-occurring illness be appropriately diagnosed and treated. Research has shown that anxiety disorders which include post-traumatic stress disorder (PTSD), obsessive-compulsive disorder, panic disorder, social phobia, and generalized anxiety disorder commonly accompany depression.
Substance use disorders (abuse or dependence) also frequently co-occur with depressive disorders. Research has revealed that people with drug and/or alcohol addiction are almost twice as likely to experience depression.
Depression has been found to occur at a higher rate among people who have other serious illnesses such as heart disease, stroke, cancer, HIV, diabetes, and Parkinson’s.
Causes of Depression
Very often, a combination of cognitive, genetic, and environmental factors is involved in the onset of depression. Modern brain-imaging technologies reveal that, in depression, neural circuits responsible for the regulation of moods, thinking, sleep, appetite, and behavior fail to function properly.
In some families, depressive disorders seem to occur generation after generation; however, they can also occur in people with no family history of these illnesses. Genetics research indicates that risk for depression results from the influence of specific multiple genes acting together with non-genetic factors.
Environmental factors such as trauma, loss of a loved one, a difficult relationship, financial problem, or any stressful change in life patterns, whether the change is unwelcome or desired, can trigger a depressive episode in vulnerable individuals. Once someone experiences a bout of depression later episodes of depression may occur without an obvious cause.
Men and Depression
Men are more likely than women to report alcohol and drug abuse or dependence in their lifetime; however, there is debate among researchers as to whether substance use is a “symptom” of underlying depression in men or a co-occurring condition that more commonly develops in men. Nevertheless, substance use can mask depression, making it harder to recognize depression as a separate illness that needs treatment.
Instead of acknowledging their feelings, asking for help, or seeking appropriate treatment, men may turn to alcohol or drugs when they are depressed, or become frustrated, discouraged, angry, irritable, and, sometimes, violently abusive. Some men deal with depression by throwing themselves compulsively into their work, attempting to hide their depression from themselves, family, and friends. Other men may respond to depression by engaging in reckless behavior, taking risks, and putting themselves in harm’s way.
02 Wednesday Nov 2022
Posted in brain, Coping Skills, Depression
≈ Comments Off on Self-Care for Depression
Tags
As a clinical psychologist, Mary Pipher, PhD, designed “healing packages” for her patients: activities, resources, and comforts to help them recover from trauma. Then, after Dr. Pipher’s book Reviving Ophelia became a runaway best-seller, she herself suffered from an episode of major depression and designed a healing package of her own. “The essence of my personal healing package,” she describes in her book Seeking Peace, “was to keep my life as simple and quiet as possible and to allow myself sensual and small pleasures.” She created a mini-retreat center in her home and modified the ancient ways of calming troubled nerves to fit her lifestyle. Pipher’s healing package looked like this:

She accessed the healing power of water by walking at Holmes Lake Dam, swimming at the university’s indoor pool, and reading The New Yorker magazine in the bathtub every morning.
She cooked familiar foods, dishes that reminded her of home: jaternice, sweetbreads, and perch; and cornbread and pinto beans with ham hocks.
She unpacked her childhood teacup collection and displayed it near her computer desk to remind her of happy times and of people who loved her.
She reconnected with the natural world by walking many miles every week on the frozen prairie, watching the yellow aconites blossom in February and the daffodils and jonquils in March, following the cycles of the moon, and witnessing sunrises and sunsets.
She read biographies of heroes like Abe Lincoln, and read the poetry of Billy Collins, Robert Frost, Mary Oliver, and Ted Kooser.
She found role models for coping with adversity.
She limited her encounters with people and gave herself permission to skip holiday gatherings and postpone social obligations. She erased calendar engagements until she had three months of “white space” in her future.
She embraced her body through yoga and massage. She started to pay attention to tension in her neck and other cues from her body and let those signals teach her about herself.
She meditated every day.
These activities were exactly what she needed to emerge from the other side of depression. She writes:
“After taking care of my body for several months, it began to take good care of me. My blood pressure improved and my heart problems disappeared. After a few months of my simple, relatively stress-free life and my healing package of activities, I felt my depression lifting. I enjoyed the return of positive emotions: contentment, joy, calmness and new sparks of curiosity and energy. I again felt a great tenderness toward others.”

Psychiatrist James Gordon, MD, discusses similar healing packages in his best-selling book Unstuck. At the end of his first meetings with all of his patients, he will write out a “prescription of self-care,” which includes instructions on changing diet, advice about specific recommended meditations or exercises, and a list of supplements and herbs. “Among my recommendations, there are always actions, techniques, approaches, and attitudes that each person has told me — which she already knows — are helpful,” he explains. At the end of his introduction, he suggests each reader take some time to write out his or her own prescription. He supplies a form and everything.
Each person’s healing package is unique. Many people have benefited from more meditation and mindfulness exercises, psychotherapy sessions, and therapies like Eye Movement Desensitization and Reprocessing (EMDR) that help unclog the brain of painful memories. Some people do better with more physical exercise and nutritional changes. While mindfulness and meditation have certainly helped many become aware of my rumination patterns, the most profound changes in others recovery have come from the bags of dark, green leafy vegetables, yoga, and breathing exercises.
It’s empowering to know that we don’t need a doctor or any mental health professional to design a healing package for us. We are perfectly capable of writing this prescription ourselves. Sometimes (not always), all it takes are a few simple tweaks to our lifestyle over a period to pull us out of a crippling depression or unrelenting anxiety.
08 Friday Jul 2022
Posted in Coping Skills
≈ Comments Off on Watch “This could be why you’re depressed or anxious | Johann Hari” on YouTube
Tags
29 Wednesday Dec 2021
Posted in Depression, Mental Health, Research, Uncategorized
≈ Comments Off on Depression and the inflammatory process
Tags
Most people feel down, tired and inactive when they’re injured or ill. This “sickness behavior” is caused by the activation of the body’s immune response. It’s the brain’s way of conserving energy so the body can heal.
This immune response can also occur in people with depression. This has prompted some researchers and clinicians to hypothesise that depression is actually a side effect of the inflammatory process.
But while there may be a connection between inflammation and depression, one doesn’t necessarily lead to the other. So it’s too simplistic to say depression is a physical, rather than a psychiatric, illness.
University of California clinical psychologist and researcher George Slavich is one of the key recent proponents of depression as a physical illness. He hypothesises that social threats and adversity trigger the production of pro-inflammatory “cytokines”. These are messenger molecules of the immune system that play a critical role in orchestrating the host’s response to injury and infection.
This inflammatory process, Slavich argues, can initiate profound behavioral changes, including the induction of depression.
The idea that the activation of the immune response may trigger depression in some people is by no means a new one. Early descriptions of post-influenza depression appeared in the 19th century in the writings of English physician Daniel Tuke.
But it was not until the 1988 seminal paper, published by veterinarian Benjamin Hart, that the phenomenon of acute “sickness behavior” caught the interest of the scientific community.
Hart described his detailed observations of the “behavior of sick animals”. During acute infection, and in response to fever, the animals sought sleep, lost their appetite, showed a reduction in activity, grooming and social interactions, as well as showing signs of “depression”.
Just like the immune response itself, these changes reflect an evolved survival strategy that shifts priorities toward energy conservation and recovery.
Cytokine-induced sickness behavior has subsequently been studied as an example of communication between the immune system and the brain.
The behavioral changes during sickness resemble those associated with depression, so it didn’t take long for researchers to make a connection between the phenomenon of sickness behavior and mental disorders.
Such speculation was strengthened by research showing that depressive states can be experimentally induced by administering cytokines and other immunogenic agents (such as vaccines) that cause an inflammatory response.
Depression is frequently associated with inflammatory illnesses such as heart disease and rheumatoid arthritis. It’s also a side effect of treatment with cytokines to enhance the immune system.
Over recent decades, researchers have made progress in understanding how inflammation may impact on the activity of signalling pathways to and from the brain, as well as on the functioning of key neural systems involved in mood regulation.
From the available evidence it’s clear, however, that not everyone who suffers from depression has evidence of inflammation. And not all people with high levels of inflammation develop depression.
Trajectories of depression depend on a complex interplay of a spectrum of additional risk and resilience factors, which may be present to varying degrees and in a different combination in any individual at different times. These factors include the person’s:
In line with the notion that inflammation drives depression, some researchers have already trialled the effectiveness of anti-inflammatory therapy as a treatment for depression.
While some recipients (such as those with high levels of inflammation) showed benefit from the treatment, others without increased inflammation did not. This supports the general hypothesis.
However, in our desire to find more effective treatments for depression, we should not forget that the immune response, including inflammation, has a specific purpose. It protects us from infection, disease and injury.
Cytokines act at many different levels, and often in subtle ways, to fulfill their numerous roles in the orchestration of the immune response. Undermining their vital role could have negative consequences.
The recent enthusiasm to embrace inflammation as the major culprit in psychiatric conditions ignores the reality that “depression” is not a single condition. Some depressive states, such as melancholia, are diseases; some are reactions to the environment; some are existential; and some normal.
Such separate states have differing contributions of biological, social and psychological causes. So any attempt to invoke a single all-explanatory “cause” should be rejected. Where living organisms are concerned it is almost never that simple.
In the end, we cannot escape the reality that changes must occur at the level of the brain, in regions responsible for mood regulation, for “depression” to be experienced.
12 Thursday Mar 2020
Posted in Creative Therapy Tools
Tags
In my years f doing groups I have on occasion facilitated men only groups. One issue that comes up is depression. We all have bouts of sadness now and then and when those bouts of sadness interfere with our daily lives than we need to take a step in the direction of change. Below is a handout I often use, particularly with dual diagnosed men.
Symptoms of Depression
Not everyone who is depressed or manic experiences every symptom. Some people experience only a few; some people suffer many. The severity of symptoms varies among individuals and also over time.
· Persistent sad, anxious, or “empty” mood.
· Feelings of hopelessness or pessimism.
· Feelings of guilt, worthlessness, or helplessness.
· Loss of interest or pleasure in hobbies and activities that were once enjoyable
· Decreased energy, fatigue; feeling “slowed down.”
· Difficulty concentrating, remembering, or making decisions.
· Trouble sleeping, early-morning awakening, or oversleeping.
· Changes in appetite and/or weight.
· Thoughts of death or suicide, or suicide attempts.
· Restlessness or irritability.
· Persistent physical symptoms, such as headaches, digestive disorders, and chronic pain that do not respond to routine treatment.
Co-Occurrence of Depression with Other Illnesses
Depression can coexist with other illnesses. In such cases, it is important that the depression and each co-occurring illness be appropriately diagnosed and treated. Research has shown that anxiety disorders which include post-traumatic stress disorder (PTSD), obsessive-compulsive disorder, panic disorder, social phobia, and generalized anxiety disorder commonly accompany depression.
Substance use disorders (abuse or dependence) also frequently co-occur with depressive disorders. Research has revealed that people with drug and/or alcohol addiction are almost twice as likely to experience depression.
Depression has been found to occur at a higher rate among people who have other serious illnesses such as heart disease, stroke, cancer, HIV, diabetes, and Parkinson’s.
Causes of Depression
Very often, a combination of cognitive, genetic, and environmental factors is involved in the onset of depression. Modern brain-imaging technologies reveal that, in depression, neural circuits responsible for the regulation of moods, thinking, sleep, appetite, and behavior fail to function properly.
In some families, depressive disorders seem to occur generation after generation; however, they can also occur in people with no family history of these illnesses. Genetics research indicates that risk for depression results from the influence of specific multiple genes acting together with non-genetic factors.
Environmental factors such as trauma, loss of a loved one, a difficult relationship, financial problem, or any stressful change in life patterns, whether the change is unwelcome or desired, can trigger a depressive episode in vulnerable individuals. Once someone experiences a bout of depression later episodes of depression may occur without an obvious cause.
Men and Depression
Men are more likely than women to report alcohol and drug abuse or dependence in their lifetime; however, there is debate among researchers as to whether substance use is a “symptom” of underlying depression in men or a co-occurring condition that more commonly develops in men. Nevertheless, substance use can mask depression, making it harder to recognize depression as a separate illness that needs treatment.
Instead of acknowledging their feelings, asking for help, or seeking appropriate treatment, men may turn to alcohol or drugs when they are depressed, or become frustrated, discouraged, angry, irritable, and, sometimes, violently abusive. Some men deal with depression by throwing themselves compulsively into their work, attempting to hide their depression from themselves, family, and friends. Other men may respond to depression by engaging in reckless behavior, taking risks, and putting themselves in harm’s way.
How to Help Yourself if You Are Depressed
Depressive disorders can make one feel exhausted, worthless, helpless, and hopeless. It is important to realize that these negative views are part of the depression and do not accurately reflect the actual circumstances. Negative thinking fades as treatment begins to take effect. In the meantime:
05 Thursday Mar 2020
Posted in Depression, TedTalks, youtube
≈ Comments Off on What is #depression? – Helen M. Farrell
Tags
21 Friday Feb 2020
Posted in Depression, mental health, Wellness, Yoga
Tags
From an article on the Yoga International web site: 
Anyone who has suffered from depression understands how deep, abiding sadness or worthlessness can infiltrate and affect every aspect of our being. Our psychological makeup, physical health, mental outlook, and even our ability to interact with friends and family and be present to the world around us can get shaken to their core. Why? Because we identify with and attach ourselves to things that will inevitably change. As our feelings and other symptoms of depression persist, we have an increasingly difficult time imagining a life in which we break free from their spell and avoid “becoming” them.
Yoga teaches us that we aren’t our feelings or our symptoms but live in multidimensional relationship with them. One way to grasp this paradox is to picture the Self (purusha or pure, undifferentiated awareness) as pervading all nine interlocking and interdependent spheres of influence without being any one of them. See More here.
https://yogainternational.com/article/view/yoga-for-depression-an-integrated-practice
10 Monday Feb 2020
Posted in Depression, TedTalks, YouTube
≈ Comments Off on Why We Need to Talk About Depression | Kevin Breel | TED Talks
Tags
25 Wednesday Dec 2019
Posted in Depression, Uncategorized
Tags
Whether you’re a college student in the middle of a major slump, a new mom who can’t pinpoint why she’s feeling so glum, or a retiree grieving over the loss of a loved one, that question isn’t an easy one to answer.
But there’s one thing for sure: “It is much more than just a sad mood,” said Angelos Halaris, MD, a professor of psychiatry and medical director of adult psychiatry at the Loyola University Medical Center in Chicago. Symptoms may include everything from hopelessness and fatigue to physical pain. And just as symptoms vary from person to person, so do the actual diagnoses. The word depression is actually just an umbrella term for a number of different forms, from major depression to atypical depression to dysthymia.
The most common form of depression? Major depression. In fact, about 7 percent of the adult U.S. population has this debilitating mental health condition at any given time, according to the National Institute of Mental Health (NIMH).
If you’re experiencing major depression, you may feel and see symptoms of extreme sadness, hopelessness, lack of energy, irritability, trouble concentrating, changes in sleep or eating habits, feelings of guilt, physical pain, and thoughts of death or suicide — and for an official diagnosis, your symptoms must last for more than two weeks. In some instances, a person might only experience one episode of major depression, but the condition tends to recur throughout a person’s life.
The best treatment is usually with antidepressant medications, explained Dr. Halaris, but talk therapy may also be used to treat depression. And there’s good news: An estimated 80 to 90 percent of people with major depression respond well to treatment.
About 2 percent of the American population has a form of depression that’s less severe than major depression, but is still very real — dysthymia.
Dysthymia is a type of depression that causes a low mood over a long period of time — perhaps for a year or more, explained Halaris. “People can function adequately, but not optimally.” Symptoms include sadness, trouble concentrating, fatigue, and changes in sleep habits and appetite.
This depression usually responds better to talk therapy than to medications, though some studies suggest that combining medication with talk therapy may lead to the greatest improvement. People with dysthymia may also be at risk for episodes of major depression.
A whopping 85 percent of new moms feel some sadness after their baby is born — but for up to 16 percent of women, that sadness is serious enough to be diagnosable.
Postpartum depression is characterized by feelings of extreme sadness, fatigue, loneliness, hopelessness, suicidal thoughts, fears about hurting the baby, and feelings of disconnect from the child. It can occur anywhere from weeks to months after childbirth, and Halaris explained it most always develops within a year after a woman has given birth.
“It needs prompt and experienced medical care,” he said — and that may include a combination of talk and drug therapy.
Would you prefer to hibernate during the winter than face those cold, dreary days? Do you tend to gain weight, feel blue, and withdraw socially during the season?
You could be one of 4 to 6 percent of people in the United States estimated to have seasonal affective disorder, or SAD. Though many people find themselves in winter funks, SAD is characterized by symptoms of anxiety, increased irritability, daytime fatigue, and weight gain. This form of depression typically occurs in winter climates, likely due to the lessening of natural sunlight. “We don’t really know why some people are more sensitive to this reduction in light,” said Halaris. “But symptoms are usually mild, though they can be severe.”
This depression usually starts in early winter and lifts in the spring, and it can be treated with light therapy or artificial light treatment.
Despite its name, atypical depression is not unusual. In fact, it may be one of the most common types of depression — and some doctors even believe it is underdiagnosed.
“This type of depression is less well understood than major depression,” explained Halaris. Unlike major depression, a common sign of atypical depression is a sense of heaviness in the arms and legs — like a form of paralysis. However, a study published in the Archives of General Psychiatry (now known as JAMA Psychiatry) found that oversleeping and overeating are the two most important symptoms for diagnosing atypical depression. People with the condition may also gain weight, be irritable, and have relationship problems.
Some studies show that talk therapy works well to treat this kind of depression.
Psychosis — a mental state characterized by false beliefs, known as delusions, or false sights or sounds, known as hallucinations — doesn’t typically get associated with depression. But according to the National Alliance on Mental Illness, about 20 percent of people with depression have episodes so severe that they see or hear things that are not really there.
“People with this psychotic depression may become catatonic, not speak, or not leave their bed,” explained Halaris. Treatment may require a combination of antidepressant and antipsychotic medications. A review of 10 studies concluded that it may be best to start with an antidepressant drug alone and then add an antipsychotic drug if needed. Another review, however, found the combination of medications was more effective than either drug alone in treating psychotic depression.
If your periods of extreme lows are followed by periods of extreme highs, you could have bipolar disorder (sometimes called manic depressive disorder because symptoms can alternate between mania and depression).
Symptoms of mania include high energy, excitement, racing thoughts, and poor judgment. “Symptoms may cycle between depression and mania a few times per year or much more rapidly,” Halaris said. “This disorder affects about 2 to 3 percent of the population and has one of the highest risks for suicide.” Bipolar disorder has four basic subtypes: bipolar I (characterized by at least one manic episode); bipolar II (characterized by hypomanic episodes — which are milder — along with depression); cyclothymic disorder; and other specified bipolar and related disorder.
People with bipolar disorder are typically treated with drugs called mood stabilizers.
Premenstrual dysphoric disorder, or PMDD, is a type of depression that affects women during the second half of their menstrual cycles. Symptoms include depression, anxiety, and mood swings. Unlike premenstrual syndrome (PMS), which affects up to 85 percent of women and has milder symptoms, PMDD affects about 5 percent of women and is much more severe.
“PMDD can be severe enough to affect a woman’s relationships and her ability to function normally when symptoms are active,” said Halaris. Treatment may include a combination of depression drugs as well as talk and nutrition therapies.
Also called adjustment disorder, situational depression is triggered by a stressful or life-changing event, such as job loss, the death of a loved one, trauma — even a bad breakup.
Situational depression is about three times more common than major depression, and medications are rarely needed — that’s because it tends to clear up over time once the event has ended. However, that doesn’t mean it should be ignored: Symptoms of situational depression may include excessive sadness, worry, or nervousness, and if they don’t go away, they may become warning signs of major depression.
12 Thursday Dec 2019
Posted in Handout
Tags
In my years f doing groups I have on occasion facilitated men only groups. One issue that comes up is depression. We all have bouts of sadness now and then and when those bouts of sadness interfere with our daily lives than we need to take a step in the direction of change. Below is a handout I often use, particularly with dual diagnosed men.

Symptoms of Depression
Not everyone who is depressed or manic experiences every symptom. Some people experience only a few; some people suffer many. The severity of symptoms varies among individuals and also over time.
· Persistent sad, anxious, or “empty” mood.
· Feelings of hopelessness or pessimism.
· Feelings of guilt, worthlessness, or helplessness.
· Loss of interest or pleasure in hobbies and activities that were once enjoyable
· Decreased energy, fatigue; feeling “slowed down.”
· Difficulty concentrating, remembering, or making decisions.
· Trouble sleeping, early-morning awakening, or oversleeping.
· Changes in appetite and/or weight.
· Thoughts of death or suicide, or suicide attempts.
· Restlessness or irritability.
· Persistent physical symptoms, such as headaches, digestive disorders, and chronic pain that do not respond to routine treatment.
Co-Occurrence of Depression with Other Illnesses
Depression can coexist with other illnesses. In such cases, it is important that the depression and each co-occurring illness be appropriately diagnosed and treated. Research has shown that anxiety disorders which include post-traumatic stress disorder (PTSD), obsessive-compulsive disorder, panic disorder, social phobia, and generalized anxiety disorder commonly accompany depression.
Substance use disorders (abuse or dependence) also frequently co-occur with depressive disorders. Research has revealed that people with drug and/or alcohol addiction are almost twice as likely to experience depression.
Depression has been found to occur at a higher rate among people who have other serious illnesses such as heart disease, stroke, cancer, HIV, diabetes, and Parkinson’s.
Causes of Depression
Very often, a combination of cognitive, genetic, and environmental factors is involved in the onset of depression. Modern brain-imaging technologies reveal that, in depression, neural circuits responsible for the regulation of moods, thinking, sleep, appetite, and behavior fail to function properly.
In some families, depressive disorders seem to occur generation after generation; however, they can also occur in people with no family history of these illnesses. Genetics research indicates that risk for depression results from the influence of specific multiple genes acting together with non-genetic factors.
Environmental factors such as trauma, loss of a loved one, a difficult relationship, financial problem, or any stressful change in life patterns, whether the change is unwelcome or desired, can trigger a depressive episode in vulnerable individuals. Once someone experiences a bout of depression later episodes of depression may occur without an obvious cause.
Men and Depression
Men are more likely than women to report alcohol and drug abuse or dependence in their lifetime; however, there is debate among researchers as to whether substance use is a “symptom” of underlying depression in men or a co-occurring condition that more commonly develops in men. Nevertheless, substance use can mask depression, making it harder to recognize depression as a separate illness that needs treatment.
Instead of acknowledging their feelings, asking for help, or seeking appropriate treatment, men may turn to alcohol or drugs when they are depressed, or become frustrated, discouraged, angry, irritable, and, sometimes, violently abusive. Some men deal with depression by throwing themselves compulsively into their work, attempting to hide their depression from themselves, family, and friends. Other men may respond to depression by engaging in reckless behavior, taking risks, and putting themselves in harm’s way.
How to Help Yourself if You Are Depressed
Depressive disorders can make one feel exhausted, worthless, helpless, and hopeless. It is important to realize that these negative views are part of the depression and do not accurately reflect the actual circumstances. Negative thinking fades as treatment begins to take effect. In the meantime:

04 Wednesday Dec 2019
Posted in grounding, Health, Relaxation, Wellness
≈ Comments Off on Relaxation
Tags

Currently, there is some scientific evidence that relaxation techniques may be an effective part of an overall treatment plan for some disorders, including:
Relaxation involves practice and willingness to fully engage in the process of relaxing. Stay tuned for some great relaxing tools.
28 Monday Oct 2019
Posted in Depression, Handout, Mental Health, Psychoeducation, Therapy
≈ Comments Off on Men and Depression
Tags
depression, men, self, symtoms, wellness
In my years f doing groups I have on occasion facilitated men only groups. One issue that comes up is depression. We all have bouts of sadness now and than and when those bouts of sadness interfere with our daily lives than we need to take a step in the direction of change. Below is a handout I often use, particularly with dual diagnosed men. 
Symptoms of Depression
Not everyone who is depressed or manic experiences every symptom. Some people experience only a few; some people suffer many. The severity of symptoms varies among individuals and also over time.
· Persistent sad, anxious, or “empty” mood.
· Feelings of hopelessness or pessimism.
· Feelings of guilt, worthlessness, or helplessness.
· Loss of interest or pleasure in hobbies and activities that were once enjoyable
· Decreased energy, fatigue; feeling “slowed down.”
· Difficulty concentrating, remembering, or making decisions.
· Trouble sleeping, early-morning awakening, or oversleeping.
· Changes in appetite and/or weight.
· Thoughts of death or suicide, or suicide attempts.
· Restlessness or irritability.
· Persistent physical symptoms, such as headaches, digestive disorders, and chronic pain that do not respond to routine treatment.
Co-Occurrence of Depression with Other Illnesses
Depression can coexist with other illnesses. In such cases, it is important that the depression and each co-occurring illness be appropriately diagnosed and treated. Research has shown that anxiety disorders which include post-traumatic stress disorder (PTSD), obsessive-compulsive disorder, panic disorder, social phobia, and generalized anxiety disorder commonly accompany depression.
Substance use disorders (abuse or dependence) also frequently co-occur with depressive disorders. Research has revealed that people with drug and/or alcohol addiction are almost twice as likely to experience depression.
Depression has been found to occur at a higher rate among people who have other serious illnesses such as heart disease, stroke, cancer, HIV, diabetes, and Parkinson’s.
Causes of Depression
Very often, a combination of cognitive, genetic, and environmental factors is involved in the onset of depression. Modern brain-imaging technologies reveal that, in depression, neural circuits responsible for the regulation of moods, thinking, sleep, appetite, and behavior fail to function properly.
In some families, depressive disorders seem to occur generation after generation; however, they can also occur in people with no family history of these illnesses. Genetics research indicates that risk for depression results from the influence of specific multiple genes acting together with non-genetic factors.
Environmental factors such as trauma, loss of a loved one, a difficult relationship, financial problem, or any stressful change in life patterns, whether the change is unwelcome or desired, can trigger a depressive episode in vulnerable individuals. Once someone experiences a bout of depression later episodes of depression may occur without an obvious cause.
Men and Depression
Men are more likely than women to report alcohol and drug abuse or dependence in their lifetime; however, there is debate among researchers as to whether substance use is a “symptom” of underlying depression in men or a co-occurring condition that more commonly develops in men. Nevertheless, substance use can mask depression, making it harder to recognize depression as a separate illness that needs treatment.
Instead of acknowledging their feelings, asking for help, or seeking appropriate treatment, men may turn to alcohol or drugs when they are depressed, or become frustrated, discouraged, angry, irritable, and, sometimes, violently abusive. Some men deal with depression by throwing themselves compulsively into their work, attempting to hide their depression from themselves, family, and friends. Other men may respond to depression by engaging in reckless behavior, taking risks, and putting themselves in harm’s way.
How to Help Yourself if You Are Depressed
Depressive disorders can make one feel exhausted, worthless, helpless, and hopeless. It is important to realize that these negative views are part of the depression and do not accurately reflect the actual circumstances. Negative thinking fades as treatment begins to take effect. In the meantime:
11 Wednesday Sep 2019
Posted in Depression, Handout, mental health, Psychoeducation, Therapy
≈ Comments Off on Men and Depression
Tags
depression, men, self, symtoms, wellness
In my years f doing groups I have on occasion facilitated men only groups. One issue that comes up is depression. We all have bouts of sadness now and than and when those bouts of sadness interfere with our daily lives than we need to take a step in the direction of change. Below is a handout I often use, particularly with dual diagnosed men.
Symptoms of Depression
Not everyone who is depressed or manic experiences every symptom. Some people experience only a few; some people suffer many. The severity of symptoms varies among individuals and also over time.
· Persistent sad, anxious, or “empty” mood.
· Feelings of hopelessness or pessimism.
· Feelings of guilt, worthlessness, or helplessness.
· Loss of interest or pleasure in hobbies and activities that were once enjoyable
· Decreased energy, fatigue; feeling “slowed down.”
· Difficulty concentrating, remembering, or making decisions.
· Trouble sleeping, early-morning awakening, or oversleeping.
· Changes in appetite and/or weight.
· Thoughts of death or suicide, or suicide attempts.
· Restlessness or irritability.
· Persistent physical symptoms, such as headaches, digestive disorders, and chronic pain that do not respond to routine treatment.
Co-Occurrence of Depression with Other Illnesses
Depression can coexist with other illnesses. In such cases, it is important that the depression and each co-occurring illness be appropriately diagnosed and treated. Research has shown that anxiety disorders which include post-traumatic stress disorder (PTSD), obsessive-compulsive disorder, panic disorder, social phobia, and generalized anxiety disorder commonly accompany depression.
Substance use disorders (abuse or dependence) also frequently co-occur with depressive disorders. Research has revealed that people with drug and/or alcohol addiction are almost twice as likely to experience depression.
Depression has been found to occur at a higher rate among people who have other serious illnesses such as heart disease, stroke, cancer, HIV, diabetes, and Parkinson’s.
Causes of Depression
Very often, a combination of cognitive, genetic, and environmental factors is involved in the onset of depression. Modern brain-imaging technologies reveal that, in depression, neural circuits responsible for the regulation of moods, thinking, sleep, appetite, and behavior fail to function properly.
In some families, depressive disorders seem to occur generation after generation; however, they can also occur in people with no family history of these illnesses. Genetics research indicates that risk for depression results from the influence of specific multiple genes acting together with non-genetic factors.
Environmental factors such as trauma, loss of a loved one, a difficult relationship, financial problem, or any stressful change in life patterns, whether the change is unwelcome or desired, can trigger a depressive episode in vulnerable individuals. Once someone experiences a bout of depression later episodes of depression may occur without an obvious cause.
Men and Depression
Men are more likely than women to report alcohol and drug abuse or dependence in their lifetime; however, there is debate among researchers as to whether substance use is a “symptom” of underlying depression in men or a co-occurring condition that more commonly develops in men. Nevertheless, substance use can mask depression, making it harder to recognize depression as a separate illness that needs treatment.
Instead of acknowledging their feelings, asking for help, or seeking appropriate treatment, men may turn to alcohol or drugs when they are depressed, or become frustrated, discouraged, angry, irritable, and, sometimes, violently abusive. Some men deal with depression by throwing themselves compulsively into their work, attempting to hide their depression from themselves, family, and friends. Other men may respond to depression by engaging in reckless behavior, taking risks, and putting themselves in harm’s way.
How to Help Yourself if You Are Depressed
Depressive disorders can make one feel exhausted, worthless, helpless, and hopeless. It is important to realize that these negative views are part of the depression and do not accurately reflect the actual circumstances. Negative thinking fades as treatment begins to take effect. In the meantime:
20 Tuesday Aug 2019
Posted in Depression, Self-Care
≈ Comments Off on Self-Care for Depression 2
Tags
Everyone gets the blues from time to time. In fact, according to the National Institute of Mental Health, major depressive disorder (also known as depression) affects 7 percent of adult Americans every year, and chronic, mild depression affects 2 percent.
The good news is you may not have to turn to drugs to combat the blues. Of course, if bouts of depression continue for weeks at a time, you need to see a health-care professional and work out a treatment plan. But for occasional down days, adopting some simple lifestyle and diet changes and making them part of your daily routine can naturally boost your mood.

A regular dose of exercise may be just what you need to ease the first signs of depression or anxiety. A study by a team of researchers including Michael Babyak, professor of medical psychology at the Duke University Medical Center, showed that engaging in mild aerobic exercise three times a week was as effective as undergoing a standard treatment with antidepressant medications. While researchers aren’t sure why exercise helps, some speculate being active may affect brain chemicals or improve blood flow to the brain. Babyak says you don’t necessarily have to do extremely vigorous activity — even fast walking (try for 30 minutes at least three times a week) may help improve your mood.
The foods you choose can also affect your mood. “Low levels or actual deficiency of such nutrients as omega-3 fatty acids, zinc, selenium, chromium, vitamin D, and the B vitamins folic acid and B12 are all associated with human depressive symptoms,” says Alan C. Logan, naturopathic physician and author of The Brain Diet (Cumberland House, 2007). However, Ronald Pies, M.D., clinical professor of psychiatry at Tufts University School of Medicine and professor of psychiatry at SUNY Upstate Medical University, Syracuse, adds that there’s no solid evidence to date that specific foods or nutrients can boost a person’s mood under normal circumstances. The key, he notes, is moderation. “A nutritious, well-balanced diet is very important for maintaining a normal mood.”
Omega-3 fatty acids, found in fish, fish oils, and flaxseed, are being studied for their mood-boosting properties. Specifically, research suggests that eicosapentaenoic acid (EPA), an omega-3 found in oily fish, may be especially effective against depression. Though the jury is still out on all of the potential benefits of omega-3s, many experts say it’s worth giving them a try. “Consider adding more omega-3 fatty acids to your diet, if not to boost mood, then to improve your overall cardiovascular fitness,” says Ronald Pies, M.D., clinical professor of psychiatry at Tufts University School of Medicine and professor of psychiatry at SUNY Upstate Medical University, Syracuse. “This can be easily done by increasing your dietary consumption of certain fish, such as salmon or herring.” You can also get fish oil in supplement form.
When your body relaxes, it can help you see the world from a rosier perspective. One way to achieve effective relaxation is through the increasingly popular practice of yoga. Studies by India’s National Institute of Mental Health and Neurosciences have shown that certain yoga-linked breathing exercises can lower levels of cortisol, an adrenal hormone linked to stress. Another study found that immediately after a one-hour session, yoga practitioners had a healthy boost in levels of the mood-related neurotransmitter gamma-aminobutyric acid (GABA). Low brain levels of GABA have been associated with anxiety and depression. Yoga has many other health benefits as well.
Some people report that taking the herbal supplement St. John’s wort helps their depressive symptoms, while others find no benefit. Naturopathic physician and author Alan C. Logan says research has shown that it’s worth trying St. John’s wort if you have mild to moderate depression. He warns, however, that this herb shouldn’t be used if you’re already taking antidepressant medications. In addition, St. John’s wort can interact with many other prescription drugs, such as birth control pills, making them less effective. As a general rule, it’s always advisable to consult a health-care practitioner before using any nutritional supplement.
Getting your feelings out, be it in a letter or journal entry, or through creative writing, can provide insight into your feelings and give you perspective on how to let go of destructive emotions. James W. Pennebaker, Ph.D., professor and chair of the department of psychology at the University of Texas, says that although research about the value of expressive writing is still preliminary, regularly recording your emotional upheavals can improve both your physical and mental health. He recommends a writing session that lasts for a minimum of 15 minutes a day, on paper or the computer, for at least three or four consecutive days. Try to write continuously without worrying about spelling or grammar.
Research shows that a lack of sunlight during the dark winter months can cause a verifiable condition called seasonal affective disorder (SAD), or the winter blues. Alan C. Logan, naturopathic physician and author, says that even adults who don’t have SAD often report a decline in mood during this time. Greater exposure to natural sunlight can help combat this problem, as can the regular use of a full-spectrum light box. “The value of a light box has also been demonstrated even in healthy adults without SAD,” says Logan. Using the light box early in the morning (7 a.m. or earlier) may be most effective, he adds.
A massage by a skilled practitioner is not only rejuvenating for your muscles, it can also be a great stress and anxiety buster. A 2005 review of many research studies showed that massage therapy consistently lowered levels of the stress hormone cortisol in patients with various physical and psychological conditions. At the same time, it increased the activity of pleasure-related chemicals in the brain. Even if it’s not for therapeutic purposes, a massage can be enjoyable and decrease muscle and mental tension.
Trying to think positively, even during down times, can also affect your mood. Start by making a list of all the things in your life that you appreciate — the results may surprise you. Alan C. Logan, naturopathic physician and author, adds that being mindful (staying in the moment) can also help. He suggests you can do this by paying attention to your thoughts, emotions, and bodily sensations. “Taking stock of these mental events in a nonjudgmental way allows for the identification of negative patterns that can lead to depressive symptoms,” he says. “Research suggests that mindfulness may lead to resilience against stress and positively alter brain activity in the areas governing emotions.”
Though your tendency may be to avoid people when you’re feeling down, often this can just add to feelings of isolation and depression. Reaching out to people, whether you discuss how you’re feeling or not, can help. Studies show that positive social ties can significantly protect a person’s health and well-being. So try to strengthen your relationships with people around you: Propose social dates, keep in touch with friends, explore volunteer opportunities, or take a new class. If your depression makes it too difficult to do these things, you should begin by reaching out to a doctor or therapist for some help.
19 Monday Aug 2019
Posted in Depression, TedTalks, YouTube
≈ Comments Off on What is #depression? – Helen M. Farrell
Tags
13 Tuesday Aug 2019
Posted in Depression, Self-Care, Uncategorized
≈ Comments Off on Self-Care and #Depression
Tags
As a clinical psychologist, Mary Pipher, PhD, designed “healing packages” for her patients: activities, resources, and comforts to help them recover from trauma. Then, after Dr. Pipher’s book Reviving Ophelia became a runaway best-seller, she herself suffered from an episode of major depression and designed a healing package of her own. “The essence of my personal healing package,” she describes in her book Seeking Peace, “was to keep my life as simple and quiet as possible and to allow myself sensual and small pleasures.” She created a mini-retreat center in her home and modified the ancient ways of calming troubled nerves to fit her lifestyle. Pipher’s healing package looked like this:
She accessed the healing power of water by walking at Holmes Lake Dam, swimming at the university’s indoor pool, and reading The New Yorker magazine in the bathtub every morning.
She cooked familiar foods, dishes that reminded her of home: jaternice, sweetbreads, and perch; and cornbread and pinto beans with ham hocks.
She unpacked her childhood teacup collection and displayed it near her computer desk to remind her of happy times and of people who loved her.
She reconnected with the natural world by walking many miles every week on the frozen prairie, watching the yellow aconites blossom in February and the daffodils and jonquils in March, following the cycles of the moon, and witnessing sunrises and sunsets.
She read biographies of heroes like Abe Lincoln, and read the poetry of Billy Collins, Robert Frost, Mary Oliver, and Ted Kooser.
She found role models for coping with adversity.
She limited her encounters with people and gave herself permission to skip holiday gatherings and postpone social obligations. She erased calendar engagements until she had three months of “white space” in her future.
She embraced her body through yoga and massage. She started to pay attention to tension in her neck and other cues from her body and let those signals teach her about herself.
 She meditated every day.
She meditated every day.
These activities were exactly what she needed to emerge from the other side of depression. She writes:
After taking care of my body for several months, it began to take good care of me. My blood pressure improved and my heart problems disappeared. After a few months of my simple, relatively stress-free life and my healing package of activities, I felt my depression lifting. I enjoyed the return of positive emotions: contentment, joy, calmness and new sparks of curiosity and energy. I again felt a great tenderness toward others.
Psychiatrist James Gordon, MD, discusses similar healing packages in his best-selling book Unstuck. At the end of his first meetings with all of his patients, he will write out a “prescription of self-care,” which includes instructions on changing diet, advice about specific recommended meditations or exercises, and a list of supplements and herbs. “Among my recommendations, there are always actions, techniques, approaches, and attitudes that each person has told me — which she already knows — are helpful,” he explains. At the end of his introduction, he suggests each reader take some time to write out his or her own prescription. He supplies a form and everything.
Each person’s healing package is unique. Many people have benefited from more meditation and mindfulness exercises, psychotherapy sessions, and therapies like Eye Movement Desensitization and Reprocessing (EMDR) that help unclog the brain of painful memories. Some people do better with more physical exercise and nutritional changes. While mindfulness and meditation have certainly helped many become aware of my rumination patterns, the most profound changes in others recovery have come from the bags of dark, green leafy vegetables, yoga, and breathing exercises.
It’s empowering to know that we don’t need a doctor or any mental health professional to design a healing package for us. We are perfectly capable of writing this prescription ourselves. Sometimes (not always), all it takes are a few simple tweaks to our lifestyle over a period of time to pull us out of a crippling depression or unrelenting anxiety.